How common is back pain?
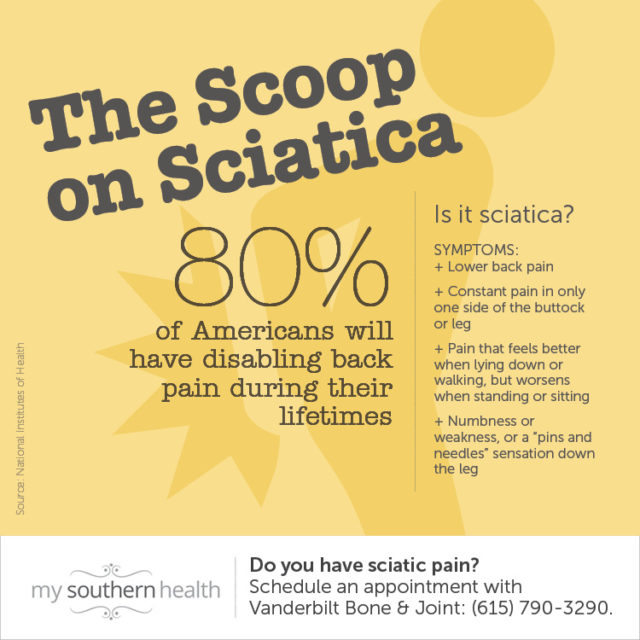
Pretty common: Most people, about 80 percent, will experience some type of back pain in their lives, according to the National Institutes of Health, and it’s one of the most common reasons people visit the doctor.
Now, for the good news: “The vast majority of back pain is not medically serious,” said Dr. Byron Schneider of the Vanderbilt Spine Center. In most cases, a physician’s role will be to help a patient get over the painful episode faster. That being said, the decision of whether to see a physician will be different for everyone and will likely depend on how much the symptoms are interfering with your ability to go about your daily activities.
When should you see a physician for back pain?
“If it’s bothering you, and you want help to see if it can be less bothersome,” Schneider said, “that’s a good reason to see a spine specialist.”
Although the following symptoms aren’t a medical emergency, Schneider recommends talking to your physician or a spine specialist if:
- You normally suffer intermittent back pain and a recent episode is lasting longer than usual.
- The pain has transitioned from being tolerable to interfering with the things you’d like to be doing.
- You’re experiencing weakness, numbness or tingling in your lower extremities.
- Pain begins shooting down your leg.
Innovative non-surgical and surgical treatments
When is surgery necessary for back pain?
Having chronic back pain does not mean someone must have back surgery. However, if ongoing back pain involves neurologic problems (for example, numbness or weakness in the arms or legs), or serious limits to what you can do physically, even after non-surgical treatment, then surgery is recommended.
Dr. Aaron Yang, a physician with Vanderbilt Spine Center, recommends discussing the option of back surgery with your doctor to see if surgical treatment might be a consideration. “That doesn’t mean a surgeon is going to operate on you right away,” Yang said. Even if your condition is targetable through surgery, a surgeon must factor in your other health conditions and the results you expect after a potential procedure, he added.
“I try to encourage patients to think of it in the greater context,” Yang said. “Can a patient live with this pain, or are they at a point where they feel like they just have to have surgery because it’s impacting them that much?”
Yang explains that it is often OK to take conservative approaches (steps that do not involve surgery) to treat back pain, and meet goals for functioning before considering surgery. Many people fear that if they don’t have surgery, their condition won’t improve or it will get worse. Numbness or weakness may also prompt patients to seek surgery sooner. But if a person can tolerate their pain and they do not have neurological symptoms, they can — and should — take their time to explore the options.
Explore more about Orthopedics & Spine

4 common myths about spine surgery

How to decide whether back surgery is the right route for you

Motion-preserving spinal surgeries can offer better recovery
What about neck surgery?
Problems with the spine and spinal cord in the neck are unfortunately quite common as well. For many people, relief comes from surgery.
Some neck surgeries involve fusing vertebrae — attaching two or more of the bones forming the spine to each other to fix a structural problem and decrease pain.
However, fusion reduces range of motion, and that in turn can create long-term side effects.
Motion-preserving surgery, however, does not artificially stiffen the spine. This makes it a good treatment both for young, active people, and for older patients because it comes with a shorter recovery period than fusion surgery and it allows full range of motion after recovery.
There are two types of motion-preserving spinal surgeries: cervical disc replacement and cervical laminoplasty (learn more about each here). Problems that these motion-preserving surgeries can solve include degenerative conditions (ones that get worse over time) that put pressure on the spinal cord or on the spinal nerve roots. Those causes can include arthritis, bone spurs, tumors, fractures, cervical myelopathy, cervical stenosis (narrowing of the spinal canal in the neck) and more.
Will spine surgery immediately fix my neck or back pain?
It depends on the patient — and their motivation.
Spine surgery involves some pre- and post-op commitment. Sometimes a person may need to lose weight, stop smoking, treat underlying conditions, or change or stop medications before undergoing spine surgery. “Taking care of those things before surgery gives you the best chance of recovering afterward and achieving the best result,” explained Dr. Scott Zuckerman, a neurological surgeon with Vanderbilt Spine Center.
Keeping up with these positive changes after surgery is important for healing and improving strength and flexibility. “Patients need a good attitude and a lot of motivation and perseverance,” Zuckerman said.